Lower Back Pain with Leg Numbness: There Is a Solution
By Manisha Wijayanayagam, Physical Therapist and Pelvic Health Provider
If you’ve ever experienced lower back pain that spreads down into your leg, along with tingling or numbness, you’re not alone—and you’re not without options. This combination of symptoms can be uncomfortable and disruptive to your everyday life. The good news is that there is a solution. With the right assessment and treatment plan, you can manage the pain and get back to doing the things you enjoy.
What Causes Lower Back Pain with Leg Numbness?
Lower back pain on its own is already a common issue, often due to muscle strain, poor posture, or injury. But when it’s accompanied by leg numbness or tingling, it can be an indicator of nerve involvement.
Here are a few of the most common causes:
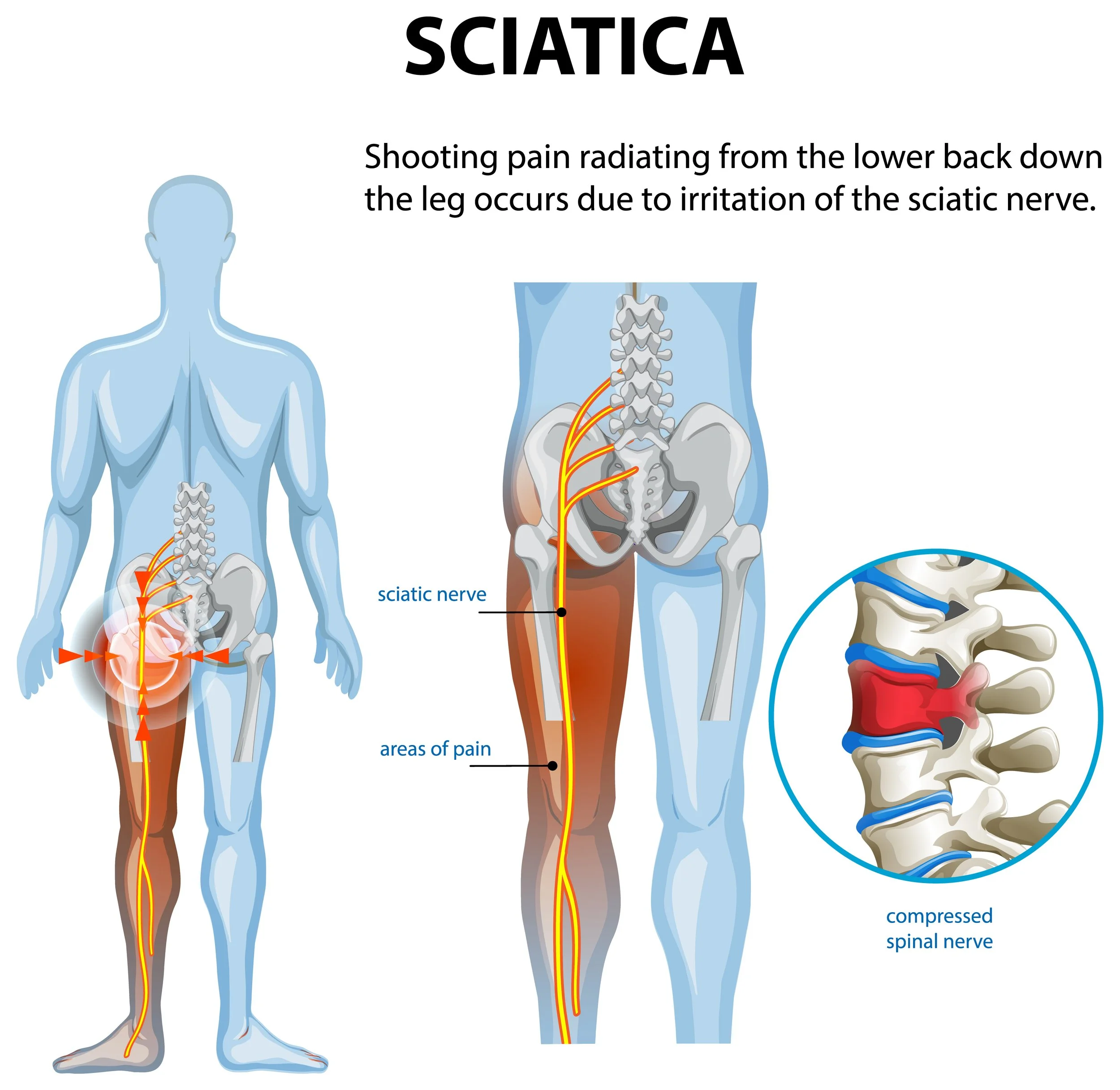
Sciatica: Sciatica is not a condition itself, but a symptom of something pressing on the sciatic nerve. It runs from your lower back, through the buttocks, and down each leg. When this nerve gets irritated or compressed, it can cause pain, numbness, or weakness in the leg, usually on one side.
Herniated or Bulging Disc: Between each vertebra in your spine are discs that act as cushions. If a disc bulges or herniates, it can press on a nearby nerve root, leading to pain that travels into the leg and causes numbness or tingling. This is one of the most common causes of sciatica.
Spinal Stenosis: This is a narrowing of the spaces within your spine, which can put pressure on the nerves. It’s more common in older adults and can cause back pain, leg numbness, and weakness, especially when walking or standing for long periods.
Piriformis Syndrome: Sometimes, the piriformis muscle in the buttocks can irritate the sciatic nerve. This condition mimics sciatica and can cause pain and numbness down the leg.
Why You Shouldn’t Ignore It
It might be tempting to wait and hope the pain goes away. And in some cases, it might. But persistent back pain with leg numbness should be checked by a healthcare professional. Ignoring it can lead to:
Worsening nerve damage
Loss of muscle strength
Difficulty walking or standing
Long-term mobility issues
How Physiotherapy Can Help
Here’s the part you’ve been waiting for: Yes, there is a solution—and physiotherapy is one of the most effective non-invasive approaches to treating this condition without surgery or long-term medication use.
1. Comprehensive Assessment
Your physiotherapist will begin by asking about your symptoms, health history, and how the pain affects your life. They will assess your posture, range of motion, nerve function, and strength to understand the root cause of your symptoms.
2. Personalised Treatment Plan
No two people are exactly the same, which is why we don’t take a one-size-fits-all approach. Based on your assessment, your physiotherapist will design a tailored program that may include:
Manual therapy – hands-on techniques to relieve pain and improve mobility
Targeted exercises – to strengthen your core, support your spine, and take pressure off the affected nerve
Stretching – especially for tight muscles like the hamstrings, hip flexors, or piriformis
Postural correction – to help reduce strain on your spine
Education – teaching you how to move safely, sit properly, and avoid flare-ups
3. Pain Management
We can also use techniques such as dry needling, electro-acupuncture, cupping, and taping to help manage pain while your body heals.
Recovery Time: What to Expect
Recovery varies depending on the cause and severity of your symptoms, but many people begin to see improvement within 4-6 weeks of consistent treatment. The key is early intervention and regular follow-up. The longer you wait, the harder it can be to resolve the issue completely.
Self-Care Tips You Can Start Today and where to find physiotherapy and chiropractic care in scarborough
While you wait for your appointment, here are a few simple things you can do:
Avoid prolonged sitting – Get up and move every 30–60 minutes.
Use good posture – Keep your back straight, shoulders relaxed, and feet flat on the floor.
Gentle stretching – Try lying on your back and bringing one knee toward your chest.
Apply heat or cold – Use heat for muscle tension or cold for inflammation.
Lower back pain with leg numbness isn’t something you have to live with. It’s your body’s way of telling you that something needs attention. Whether it’s a herniated disc, sciatica, or another condition, the sooner you seek help, the better your chances of a full recovery.
At our clinic, we’re here to help you understand the cause of your pain, treat it effectively, and prevent it from coming back. You don’t have to put up with the discomfort—there is a solution. At Cadence, we offer physiotherapy and chiropractic treatment at our Scarborough office, and we’d love to help you.